Cut claim denials and accelerate approvals through expert credentialing services. Ensure compliance, reduce delays, and improve practice revenue.
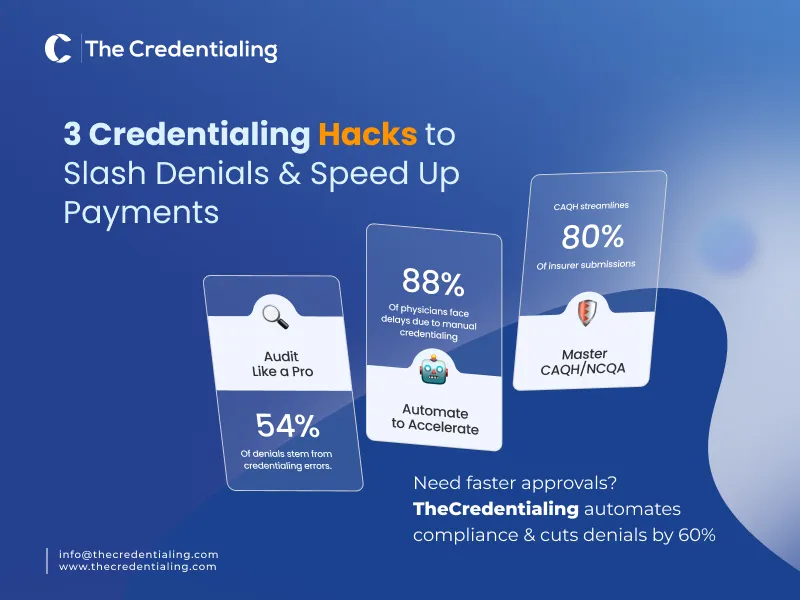
Considering that about 54% of medical practices report that provider enrollment and credentialing are the key drivers of claim denials, what’s your practice’s topmost strategy? TheCredentialing ensures experts are monitoring the process through tactics such as auditing and regular assessments of patient claims. So that the core causes of denials should be found out to not repeat the trials, leading to inefficiency of practice cash flow.
However, provider credentialing efficiency is an inadequate aspect of medical billing that paves the way for providers to have a flawless reimbursement from insurance payers. The reason? Medical credentialing and recredentialing add to the credibility and trust of practice to get timely reimbursement.
Hence, keeping updated credentials, ensuring compliance with insurance regulatory institutions, and accuracy in documentation are some key requirements. Yet, we aspire to let you learn the most trendy and effective credentialing billing services for steady approvals and reducing the rate of denials. Follow the guide to stay optimized in credentialing, leading to billing efficiency and, ultimately, to an optimized revenue cycle management (RCM).
Medicaid Credentialing Delays and the Dire Impact on Providers’ Credibility!
You may have questions like how long does credentialing take, it varies from one payer to another. The American Medical Association survey found that 88% of physicians said that the payer delays in credentialing and prior authorizations negatively impact patient outcomes.
Medicaid Credentialing taking too long to reimburse for the services or even approvals has become a burdensome task for healthcare providers to handle care. Although the standard period for a credentialing approval is 30-90 days, yet, healthcare providers face the challenge of lengthy delays. Due to the different rules of every payer and application processing speed, many claims are denied as waiting periods are lengthy.
As a result, the insurance payers hold the amount because the extension of a medical provider staying out-of-network restrains them from reimbursement.
Statistical data shows that the average rate of a claim denial is $118, and in collection, the healthcare providers lose $262 billion annually due to claim denials.
These issues accumulate over time and make billing and medical provider credentialing the most resource-draining task. So, what’s the solution? The CAQH Index reports that the healthcare industry spends $.2.76 billion annually on provider credentialing. However, automation efficiency can reduce that number. Plus, assess the key areas to support your credentialing billing such as:
- Is your Medicaid Credentialing as easy as commercial insurance enrollment?
- Do your practice providers have real-time visibility into their application status?
- Do you think that your Medicaid was held accountable for processing delays?
- Do you think that your credentialing, billing, and compliance should be handled by a single expert team?
Assess these questions and identify the root cause that could help you with the right focus and strategy. Moreover, if you are an aspirant to grow your practice smartly with the advanced tech trends, connect with TheCredentialing and go on! This is the answer if you are looking for the best credentialing billing services.
Whether the need is to have faster Medicaid approvals, lower denials, and predictable revenue, TheCredentialing is a leading platform that serves across all states of the United States with due care and automation advancement. However, never get misled by the free credentialing billing services as such claims may end you in a flawed process.
Perform a Claim Denial Assessment for a Provider Credentialing
By implementing a claim denial assessment, professionals can reach the root cause of rejection. Analyzing the denial trends will help you trace back to the incomplete or delayed credentialing. Such an assessment will help you pinpoint credentialing-related issues, including expired licenses, missing NPI numbers, and outdated payer information. For an effective claim denial assessment, there are some key points to consider:
Begin the process by identifying the common reasons, categorising them based on the common themes, and resubmitting the correct versions.
Develop a robust tracking mechanism that can monitor the denial status and ensure timely follow-up.
When you have proper mechanisms to identify the root causes, it will help you avoid denials further in the future and improve the process through steps as follows:
- Documentation accuracy is the key consideration for insurance payers.
- Coding and claim accuracy to create a solid understanding of procedures.
- Compliance with payer requirements to ensure the stability of revenue cycle and healthcare reimbursement.
TheCredentialing experts also efficiently deal with the claim denial audits to increase the billing and claim credibility. These professionals know the varying levels of challenges with each medical specialty.
Our approach is to deeply examine every document, code accurately to ensure error-free claim submission and smooth reimbursement. While reflecting on the IPD and OPD setting, we figure out and improve improper payments resulting from the incorrect categorization of medical billing codes.
Key Credentialing Platforms for Providers to Scrutinize: NCQA & CAQH
Understanding the two major systems in credentialing will help practices to run credentialing processes smoothly. For instance, the Council for Affordable Quality Healthcare (CAQH) is a non-profit alliance for health plans and trade associations that ensure a collaborative ground for many healthcare entities involved. This platform streamlines healthcare, reduces costs, and standardized the reimbursement collection procedure. Here are the key points:
- CAQH helps reduce provider burden and improve data accuracy.
- Providers don’t pay to create CAQH profiles—insurers cover the cost.
- CAQH doesn’t submit applications but allows payers to access provider files.
- Providers upload credentials like licenses and DEA certificates to CAQH
- CAQH replaced repetitive submissions to insurers with one universal system.
- The platform speeds up credentialing and reduces errors.
While CAQH stands for streamlining the payment collection, NCQA (National Committee for Quality Assurance) ensures the enhancement of the credentialing standards and accrediting healthcare organizations. In short, one ensures the quality of the credentialing process, whereas the other simplifies the process. Here are some key notes on the NCQA’s functioning:
- CAQH collects and stores provider credentials.
- NCQA sets the standards for those credentials.
- NCQA is a non-profit focused on healthcare quality.
- Hospitals and health plans use NCQA standards for credentialing.
- NCQA reviews if physician info meets quality benchmarks.
- It also sets standards for training and improvement programs.
Why Turning to Automation is a Necessity for Healthcare Providers?
Credentialing is an important process that, without the process, a provider cannot legally practice within a certain network, obtaining approvals for participation and maintaining compliance with insurance policies. However, this complex process requires efficient measures such as automation and tech support, as manual credentialing is plagued with inefficiencies.
For instance, lengthy processing times, additional administrative burden, the risk of errors, and revenue delays. Hence, automation is the key driver of credentialing and billing efficiency, which is essentially highlighted in these points:
- Automation reduces errors in data entry, and it ensures the accuracy and completeness of credentialing records.
- Automation speeds up the verification of credentials against the primary sources.
- These systems ensure compliance with regulatory requirements and industry standards.
- Automation streamlines provider enrollment and credentialing services and resultantly reduces the burden on physicians.
- Ultimately, such efficiency contributes to billing efficiency and reduces the efforts required in billing tasks.
- Automation in billing also reduces costs and improves payments to increase the practice’s cash flow.
- Since there is no need for manual labor, it leads to lower operating costs.
The Final Thoughts: What Does the Future of Credentialing Billing Bring in Healthcare?
The future of credentialing billing in healthcare brings more advanced trends due to the advancement in credentialing and billing challenges across the industry. Automation and artificial intelligence (AI) lead credentialing and billing efficiency by streamlining effort-taking tasks, improving process accuracy, and bettering revenue cycle management.
Yet, it is not the be-all and end-all solution. Medical practices will look forward to the experts handling the advanced tools and technologies to reduce the risks and get the full benefit out of the tech efficiency.
Despite adding convenience in the credentialing and billing, certain challenges such as data privacy and security, integration with existing systems, and maintaining quality are just some of the emerging concerns with other key considerations.
However, when experts like TheCredentialing support is at your back, your practice will never risk compromises on data security, inaccurate processes, or compliance issues. We are an all-inclusive platform to support and enhance your provider credentialing with key tactics and full attentiveness.
These professional partners are just around the corner when you type credentialing services near me. Moreover, optimize your search for credentialing billing services cost as we offer a reasonable adjustment while customizing the process.