Maximize reimbursements with stress-free credentialing & billing compliance. Reduce denials, accelerate payments, and ensure seamless revenue cycle management.
Credentialing and billing are the key components of healthcare revenue cycle management (RCM). While billing ensures healthcare providers are fairly reimbursed from insurance payers and patients, the professional provider credentialing process keeps the credibility and trust of providers for insurance companies that streamline claim reimbursement.
Yet, billing accuracy and compliance are a must in these processes to maximize reimbursement and smooth RCM in health care. Healthcare providers lose up to $125 billion annually as a result of medical billing compliance issues. Plus, inefficient credentialing causes practices and 80% of denials, a significant setback for the revenue cycle.
However, focusing on key updates and billing trends may help you get a win-win in such key practices of healthcare RCM. Explore this article that highlights strategies for stress-free credentialing and billing compliance. Moreover, you will learn how medical billing and coding regulations affect reimbursement.
Credentialing and Reimbursement Rates: Understanding the Crucial Hookup!
The credentialing process for providers is the key determiner of healthcare reimbursement since it contributes to the provider’s credibility and recognition for insurance companies.
When a healthcare provider is correctly verified in their qualifications and other required criteria, insurance companies trust their performance while it increases their ability to perform care and accurately bill patients for services.
Hence, there’s little room for errors in claim generation and documentation that can disrupt the payment flow and, eventually, the practice revenue. However, for insurance providers to streamline claim payment, providers must ensure the proper course of action to ensure flawless approvals and timely reimbursement.
In contrast, credentialing issues can significantly impact the provider’s credibility and practice reputation in the long run. Moreover, there are increased chances of setbacks in the practice of financial health. Hence, professionals must accept that only conducting the optimal steps in the process of medical credentialing can bring the right results to maximize reimbursement.
Ensuring Compliance in Billing: How To Avoid Costly Errors in Medical Billing
The medical billing process is a key aspect of healthcare practice revenue cycle management (RCM). However, ensuring compliance with medical billing regulations is the prime responsibility of billers to ensure claims are submitted timely, the information is accurate, and the operations are error-free to avoid unnecessary charges, leaving the practice vulnerable to liability.
The purpose is to help medical providers ensure the protection of patient rights and access to care, eliminate fraud, and drive fair medical billing practices. Yet, the right medical staff credentialing helps practices to effectively integrate with such compliance rules. Below are the key notes on the reimbursement compliance in healthcare to implement:
Office of Inspector General (OIG)
- This regulatory body oversees programs coming through the HHS (US Department of Health & Human Services)
- Ensure healthcare organisations comply with HHS programs.
- Help to protect patient privacy and eliminate fraud while keeping patient care in line.
Healthcare Information Portability & Accountability Act (HIPAA)
- Enforces industry-wide processes and standards to ensure patient safety.
- Help providers protect sensitive patient health information.
Affordable Care Act (ACA)
- Mandates that healthcare providers adopt ethics and compliance programs to get reimbursement.
- This is under federally funded healthcare programs
- Specifies the seven key elements for healthcare organisations to follow.
- Ensure the compliance program is effective as the OIG guides on best practices.
What Billing Errors Can Impact Your Finance?
If you are concerned about how can reimbursement issues affect a medical practice, below are key notes:
Documentation and Verification Errors
Make sure accuracy is at the core when verifying patient essentials, including personal data, to ensure smooth claim processing, as a single error can cause your practice significant denials. Focus on these key points:
Clarify the insurance details, medical necessity documentation to reduce administrative headaches.
Make sure a claim does not lack medical necessity documentation, leading to significant audits.
These processes require the following:
- Diagnostic imaging (e.g., MRI, CT scans) for insurers may require proof of symptoms before approval.
- Elective surgeries for even the medically required procedures, may be denied without supporting documentation.
- Specialists’ referrals for insurance plans require pre-authorization and detailed notes to justify specialist care.
Insurance Claims Submission Errors
Make sure your practice revenue is tied to the level of accuracy and timeliness of claims submission. The mistakes, like late submissions, duplicate claims, and unverified insurance coverage, can cause denials, payment delays, and even lost revenue. Consider the points as follows:
- Each insurance company has a varying strict set of requirements.
- Practices failing to track deadlines experience cash flow disruptions.
- Timely claim submission matters in the process to avoid the hassle.
- Medicaid and Medicare have more strict filing deadlines than that of private insurers.
Duplicate billing in healthcare is also a significant default when the claim is submitted multiple times for the same services. It can lead to overpayments, denials, and even an extended administrative workload. The common causes of these errors are manual entry errors, lack of communication between front-office and billing teams. Moreover, failure to verify the insurance coverage in medical billing is also a cause of denials and other issues.
Errors in Patient Billing and Collections
Your practice patients are the key source to get the clear billing statements. Make sure they are receiving the correct billing. The insurance company can delay your payment due to misspelled figures, such as incorrect account number or visit. Moreover, incorrect charges or unclear explanations may also pose issues. Unclear medical bills also cause disputes as the patients may refuse payments, delay treatment or ignore bills that seem confusing. In these situations, your practice should consider:
- Patients must understand their financial responsibility.
- Clear billing statements reduce the likelihood of surprise billing for patients.
- Upfront cost estimates improve pateint satisfaction while building trust and transparency.
Compliance and Regulatory Violations
Make sure you are preventing your practice from HIPAA violations to secure patient information. Violations can result in significant breaches, such as severe financial penalties, legal action, and lost patient trust. Moreover, the security risks like transmission of records without encryption, sending patient details to the wrong recipient, and allowing unauthorized access to sensitive billing information.
The billing process also requires the use of modifiers to ensure the record of additional information. However, incorrect use of modifiers causes issues such as delays, denials, and reimbursement and audits.
Credentialing-related Denials Impacting the Practice Finance: What are the Billing Care Solutions?
Considering the interrelation between billing and credentialing in healthcare revenue cycle management, not only the practice billing but credentialing errors also significantly disrupt the financial cash flow. Below are the noticeable points:
Data Integrity Issues
Errors such as National Provider Identifier (NPI) numbers, tax IDs, or mispelled names can be the cause of denials.
Solution: Regularly verify and update provider information to maintain accuracy.
Non-Compliance with Payer Protocols
Provider enrollment and credentialing requirements vary across different payers.
Failure to adhere to these guidelines may also lead to denials.
Solution: Stay updated with each payer’s documentation standards and procedural policies.
Authorization and Precertification Delays
Missing or delayed authorizations for services requiring pre-approval may also cause denials.
Solution: Ensure clear procedures for obtaining and documenting necessary authorizations.
Expired or Insufficient Credentials
Providers with outdated licenses or certifications risk claim denials.
Solution: Conduct regular audits and manage credential expirations and renewals through setting reminders.
Duplicate Submissions
Duplicate claim submissions or enrollment applications also trigger automated claim denials.
Solution: Train your staff to identify duplication before claim submission for claim denial prevention.
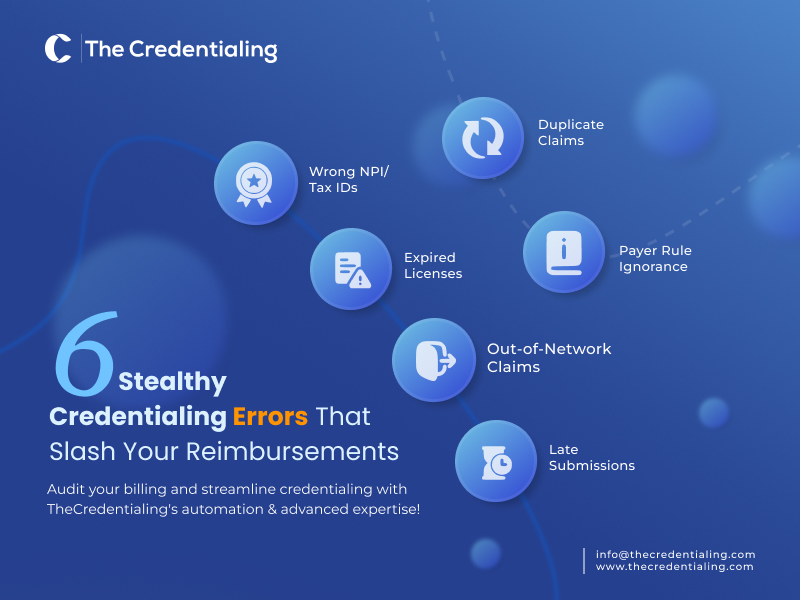
Out-of-network Provider Claims
Claims for services provided by out-of-network providers frequently get denied.
Solution: Correctly list the providers within the payer network and verify network status regularly through the provider credentialing checklist.
Missed Submission Deadlines
Each payer has a specific timeframe for claim submission.
Failure to adhere to the deadlines can also lead to denials.
Solution: Establish strict protocols and use the tracking system to monitor and adhere to submission deadlines.
Expert Medical Billing Errors to Ensure Compliance and Maximize Reimbursement
Below are the key areas of review for billing and reimbursement:
Prevent Rejection in the First Place
To get optimal reimbursement, medical practices must focus more on denied or rejected claims. Many of the factors can lead your practice to denials, yet ensuring accuracy in billing and coding will help in avoiding most common errors. Review documentation clearly on learning how to use codes properly, and understand how to determine medical necessity. For this, you can work with clients extra time to save time and prevent denials for the future.
Your Practice Needs Real-time Electronic Claim Submission
In the era of technology, waiting for long hours in claim verification and checks doesn’t hold weight. Implement electronic methods for claims verification and submission that will save you time. Electronic claims submission is a ready-made perk for medical care providers as it saves time along with providing process efficiency while reducing the chances of errors.
Use Claim Tracking and Follow-up Tools
Having effective tools for tracking claim status and follow-up is a must to meet the ever-changing coding and billing rules. These tools will provide extra checks and balances to identify discrepancies, broken rules, coding errors, and false duplicates. Using such tools will help your practice avoid denials and stay ahead in obtaining fair reimbursement.
Ensure Your Practice Has a Dedicated Medical Billing Specialist
Medical billing and coding specialists or medical credentialing companies are experts in practices to ensure the efficiency of billing. These specialists can reduce the risk of costly errors. Plus, their experience in tasks like procedure coding and billing ensure quick identification of incorrect coding, flag discrepancies in patient data, and ensure timely and accurate reimbursement for healthcare providers.
Electronic Health Records (EHRs) to Reduce Errors
EHRs can significantly address the complexity of medical billing and coding as these software can avoid errors and streamline the information flow, and improve visibility. Since all patient data is available on a single platform, healthacre providers and billing companies can reduce turnaround times on deadlines and boost claim reimbursement accuracy.
Audit your Billing and Streamline Credentialing with TheCredentialing Automation & Advanced Expertise!
TheCredentialing is reputed to be among the best credentialing companies. Get your practice regularly audited by our dedicated experts in medical billing and credentialing services. Our structured auditing and verifications will keep your billing practice clean and free of errors, leaving no room for denials. With our effective auditing, your practice will have no compromise on delays or late submissions, but we guarantee the growth of your practice and patient satisfaction.
As for credentialing efficiency, we ensure a safe bet with our digital software to streamline each step of your credentialing, such as smooth application to timely approvals. Easily track your application and credentialing while staying compliant with the regulations. Our systems integrate with the CAQH management to ensure your credentials are secure and to update your insurance network and patient base.





