Are provider enrollment and physician credentialing the same thing? Lies in the depth of these processes’ focus, function, and value. To address the confusion for now, these processes, despite being interrelated, aren’t the same in healthcare.
Provider enrollment overlaps with physician credentialing as a consolidating step to finalise the broader aspect of healthcare revenue cycle management (RCM), registering the physician with payers like Medicare, Medicaid, and commercial insurers to standardise care and reimbursement for the services delivered.
Physicians’ enrollment with multiple insurance networks enables billing patients and claiming reimbursement. Thus, both of these processes are crucial for RCM and ensure patient trust and overall experience. Yet, understanding the difference between provider enrollment and credentialing is the key to maintaining the practice workflow and reducing errors, which can become the key causes of revenue disruptions.
What is provider enrollment in healthcare & how does it work?
Provider enrollment in healthcare refers to the registration process for a healthcare provider, which can include entities like a physician, nurse practitioner, and the facility itself. Enrolling these practitioners with insurance payers such as Medicare, Medicaid, and commercial insurers is subject to receiving reimbursement for medical services rendered.
The provider gets recognition with the insurance network through this crucial step so that they can bill patients and insurance companies and get paid for their services.
The key steps in this process are to submit the detailed information about the florida medicaid provider enrollment, practice location, and tax ID, along with the work licensure. However, CAQH ProView plays a crucial role in this respect as a widely used platform that stores standardised provider data for multiple payer organisations. Although using this platform simplifies submission yet many payers require a specific application and verification.
The example includes PECOS, especially designed to manage Medicare Enrollment, while Medicaid and private insurers use their own portals. Such platforms make provider enrollment a successful process, or else, providers cannot bill insurers, which results in revenue delays and claim denials. Overall, the provider enrollment is a foundational step in revenue cycle management (RCM) to ensure compliance with regulatory bodies.
Below are the key steps:
- The provider must complete the application detailing their practice location, services provided and insurance coverage. They may also need to provide data regarding licensure, malpractice insurance, and education and training medicaid provider enrollment status.
- The credentialing organisation conducting the enrollment reviews the application and supporting documentation to determine whether the provider’s data meets participation standards.
- When the organisation ensures the provider’s credentials meet the required standards, it approves the provider’s participation in the insurance network.
What is the meaning of physician credentialing in healthcare & how does it work?
Physician credentials in healthcare support verification of the healthcare provider, such as for their qualifications, education, training, licensure, board certifications, work history, and references. By implementing such a strict assessment, the healthcare stakeholders ensure that care providers meet the established standards of care and are legally and clinically qualified to provide patient treatment.
The key steps of the process include verification of graduation from accredited medical schools, confirming valid state licensure, board certification reviews and checking peer references.
What is more important is that a professional provider credentialing process confirms privileging that authorises a physician for specific procedures and services to perform within a healthcare facility. Privileging is a crucial aspect of healthcare, maintaining quality assurance and patient safety across hospitals and clinics, it prevents potential harmful situations while promoting positive patient outcomes.
Unlike provider enrollment, which links the provider to insurance payers for billing and reimbursement, humana provider enrollment focuses solely on validating a provider’s competency. While enrollment is payer-specific and revenue-related, credentialing is clinical and internal, required for providers to deliver care within a facility and maintain accreditation with regulatory bodies.
The key steps of the process include:
- The physician maintains an application that details their education, training, and licensure. Plus, they may also need to provide data regarding their practice location, services provided, and insurance coverage.
- So, if you are concerned about whether the physician and a provider are the same thing, they aren’t always, though they overlap at times. A Physician is a medical doctor (MD or DO). Whereas, a provider refers to a broader term that encompasses many types of healthcare professionals offering care and services.
- Provider Enrollment Specialist verifies the information through contacting licensing boards, educational institutions, and other primary sources.
- The organisation reviews the provider’s application, supporting documents to determine whether these professionals meet the standards of network participation.
- In case their data meets the standards, physicians get approved to work with the insurance network.
Key Differences Between Enrollment, Credentialing, and Contracting
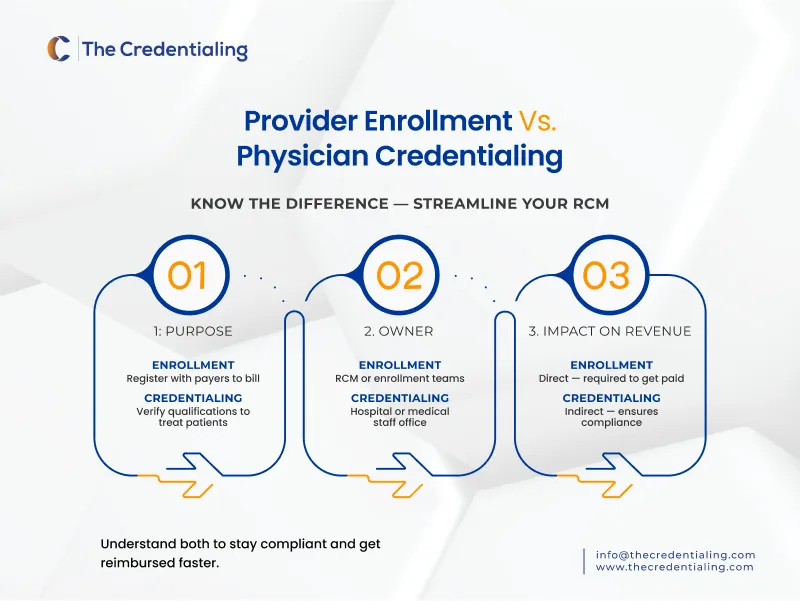
The difference between provider credentialing and enrollment lies in their factors, such as what’s the purpose of each process, documentation requirements, process owner, and more. Assess the breakdown below and also the difference between provider contracting and provider enrollment status.
| Feature | Credentialing | Provider Enrollment | Provider Contracting |
| Purpose | Verify provider qualifications & competency | Register the provider with insurance payers for reimbursement | Establish a legal and financial agreement between the provider and the payer |
| Process Owner | Medical staff office, credentialing departments | Provider enrollment or revenue cycle teams | contracting/legal departments or payer contracting units |
| Timeline | Typically 60–120 days | 30–90 days (varies by payer) | Varies by contract; 30–90+ days |
| Documentation Required | Licenses, education, board certifications, DEA, malpractice coverage | Credentialing data, CAQH profile, NPI, W-9, state licenses | Fee schedules, TIN, contract terms, credentialing and enrollment documentation |
| Outcome | Provider is approved to practice and granted privileges | Provider is enrolled in payer systems and can bill | Provider is legally contracted and reimbursed at agreed rates |
| Renewal Frequency | Every 2–3 years (based on facility or payer) | Based on payer policies (e.g., revalidation every 3–5 years for Medicare) | As per contract terms (can be multi-year with renegotiation clauses) |
| Impact on Revenue | Indirect – required for care delivery & compliance | Direct – required for claims submission and reimbursement | Direct – determines payment terms, reimbursement rates |
Single Source of Truth in Provider Credentialing: The Assumption or Reality?
Problems like redundancy and data inconsistency may be solved with a single source of truth in provider credentialing. Yet, the concept is just an assumption rather than a reality in healthcare. Single Source of Trust (SSoT) in credentialing is more of a strategic goal than a fully realized reality in many healthacre settings.
The reasons are many, and commonly occurring challenges in provider credentialing. For instance, the need for many re-checks of provider data when they want to work in different healthcare settings and separate payers causes frustration among the professionals since the same data is verified multiple times.
This delays the credentialing process. Hence, SSoT can shift this dynamic while collecting the necessary data from nationally recognised, verified sources, previous employers, medical schools, licensing boards and other sources. Storing such vast data into a single accessible platform will eliminate the repetitive verifications, lengthy paperwork and wasted time for providers and credentialers.
However, though there is a significant need to centralize the credentialing data, the actual implementation of SSoT is far from practical due to certain restrictions. For instance, fragmented systems that vary payer requirements and inconsistency of data entry practices. Yet, the rise of interoperable credentialing platforms and integrations with tools like CAQH drive the possession of a reliable SSoT, which will become more feasible.
Credentialing industry mentors are increasingly investing in the cloud-based automated systems that can reduce duplication of information and errors in the process. Thus, SSoT is rapidly moving from the aspiration to operational necessity despite not being universally achieved yet.
Career Roles & Tools in Credentialing & Enrollment
Credentialing and enrollment both play a key role in stabilizing the care delivery with fair rates of reimbursement in healthcare Revenue Cycle Management (RCM). However, provider enrollment and credentialing jobs vary in their roles and income. Credentialing specialists who verify provider qualifications and enrollment coordinators who handle payer applications and maintenance are a necessary part of the process.
There are job roles for the CAQH administrators who manage the centralized provider data systems. The U.S Bureau of Labour Statistics (2025) reports that the average salary of these professionals ranges from $50,000 to $72,000 per year.
There is a rising demand for such projects as regulatory complexity and staffing issues increase. Healthcare needs skilled partners that can pay attention to detail, have knowledge of payer systems, and have experience with credentialing software.
These career roles are essential since there is a need for accurate credentialing and enrollment processing that directly affect the timely reimbursement, compliance, and provider onboarding. Choose your top pick while navigating the varying career roles in credentialing and enrollment in healthcare.
TheCredentialing Simplifies Provider Enrollment & Credentialing for the Lasting Advantage
TheCredentialing is an innovative partner that offers hassle-free, expert, and reliable credentialing with a 98% success rate for all healthcare specialists, including Medicare & Medicaid, commercial or private. We offer a variety of credentialing processes and enrollment, compliance, and revalidation.
Going a step further into the advanced tech-driven landscape, TheCredentialing serves you with the automated credentialing portal for a hassle-free credentialing application, documentation, and payment. Save your time while reducing administrative work.
The Credentialing digital systems will keep your credentialing compliant and efficient while overcoming the many hurdles, such as high rejection rates and delays. Working only to improve your credentialing and getting you enrolled with the reputed insurance network is the goal we are working towards.