Prevent revenue loss with expert credentialing and medical billing solutions. Streamline processes, reduce denials, and boost reimbursements with automation.
The evolving phase of healthcare practice is focused on a patient-centric approach, along with care and billing management through automation. Such an approach requires healthcare professionals to stay advanced with patient-centric trends in billing, like clear and transparent communication, integration with AI-driven automation, and streamlined credentialing.
However, the latter is more crucial since it ensures the providers can adapt to these evolving trends. Credentialing concerns verifying healthcare providers’ credentials to ensure safe patient care and billing. Hence, negligence is never compromised. Otherwise, there is an increased chance of denials and financial disruptions.
Expert medical billing and credentialing services ensure that the providers effectively take care of each step of patient billing and insurance. Inefficiencies, on the other hand, lead practices to significant revenue losses.
For instance, the statistics show that up to 25% of revenue is lost due to credentialing delays, denied claims, and billing errors. Moreover, inefficiencies in medical credentialing cause 35% of healthcare organizations’ financial losses due to late reimbursement from insurance companies.
So, what’s the solution to these issues disrupting RCM practice and overall reputation? Staying aware of the factors causing disruption and following the expert-driven credentialing solutions to limit revenue leaks and optimize cash flow. Explore with us the novel trends from automation in the professional provider credentialing process to AI-integrated expert billing services in healthcare.
Stop compromising on your practice revenue leaks, leading to lengthy debts, and ensure streamlined operations for increased profitability.
Understanding the Revenue Leakage and Common Causes!
Revenue leaks in healthcare organizations refer to the difference between the provider’s supposed revenue and the collected revenue. The leaks are not instant or massive; rather, the slow cracks in cash flow are often unnoticeable, resulting from the many discrepancies in medical billing.
The issue occurs when the insurance payer or patient does not pay the agreed-upon amount due to several reasons. Recovery is possible, but with a high level of efficiency, it only helps professionals limit the leaks, not completely stop them from happening.
Moreover, healthcare organizations face billions of dollars in losses due to revenue leaks annually and cannot grow in cash flow, invest in technology, and hire specialized staff to maintain the revenue cycle management. Hence, digging out the core causes is the key to addressing the issue.
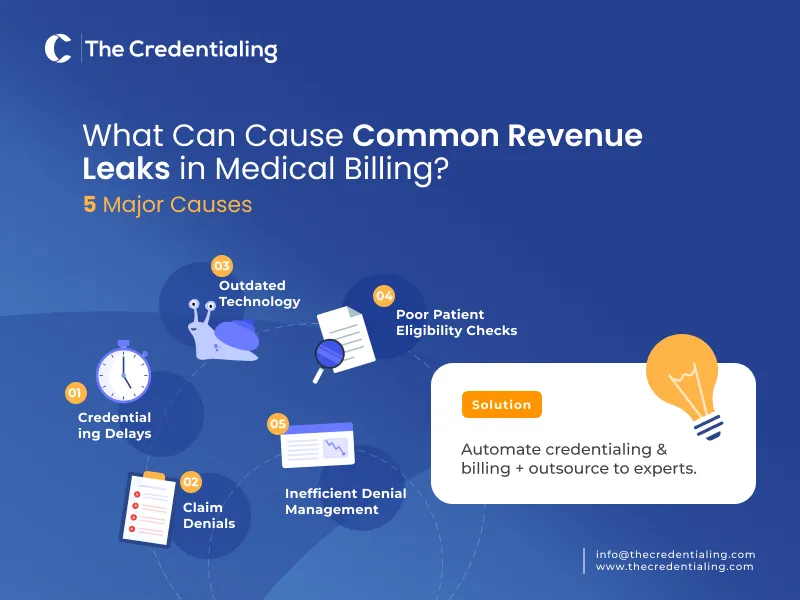
What Can Cause Common Revenue Leaks in Medical Billing?
Below are some significant areas to consider improving in:
- Inaccuracy or incomplete billing information in healthcare may significantly lead to revenue leakage.
- Incorrect coding for procedures, diagnoses, and services also significantly leads to lower reimbursement.
- Slow payment processing can also cause cash flow issues or revenue loss.
- Inadequacy of documentation also adds to the issues of coding and reimbursement.
- Lack of effective patient eligibility and insurance verification also causes denials and lost revenue.
- Poor patient communication and billing practices also lead to patient dissatisfaction and reduced future business.
- Inaccuracy or incomplete patient data also leads to billing errors and delays.
- Outdated technology usage can also slow down practice efficiency and lead to billing errors.
- Patients may move to other healthcare practices when they find an unsatisfactory billing experience.
Protecting Practice Revenue with Effective Provider Credentialing
If you are wondering why credentialing is important, it is the key component of the entire RCM matter of healthcare finance. Healthcare revenue cycle management (RCM) optimization leads to guaranteed financial stability. However, medical provider credentialing is the key aspect of the process since it verifies the provider’s qualifications to manage care and billing while staying compliant with regulations. This is how the credentialing process for providers keeps the practice’s revenue in line with patient satisfaction:
- Credentialing ensures compliance while helping practices hire certified care providers to support safe patient care and reduce the risk of audits and penalties.
- Credentialing maintains patient trust since it verifies the provider’s legitimacy to deliver safe, legal, and effective patient care.
- Credentialing helps in expanding the patient base and enrollment with an extended insurance network.
- An expanded patient base brings increased chances of revenue, and improper credentialing leads to a limited number of patients and insurance plans to accept.
- Effective credentialing processes save professionals’ time by reducing the likelihood of appeals and claims resubmission.
- The evolving phase of the healthcare industry calls for varying credentialing requirements due to changing patient and payer conditions.
- Effective credentialing processes ensure adherence and compliance with the changing industry environment for medical billing.
Credentialing efficiency is due to ensure healthcare providers are adequately performing care and other tasks related to billing. Yet, many challenges are frequent in the process, leading to financial instability.
For instance, the common issues that the providers experience in credentialing are the time-consuming nature of the process, complex compliance requirements, and added administrative burden. However, navigating the key trends in practice can ensure success in the delivery of clean claims to insurance, coding, and efficient best medical billing services.
Save valuable time by contracting with a specialized credentialing firm such as TheCredentialing, the Credentialing company for physicians. These experts will effectively manage your practice and provider credentialing while your administration will dedicatedly focus on other pressing tasks.
What Medical Billing Challenges Lead Practices to Revenue Leakage?
Not only the issues in credentialing but also medical billing challenges become hurdles for practices, causing cash flow leaks. Professionals should be wary of some of the significant errors in billing.
For instance, inaccuracy and missed patient and medical information are at the top, leading to claims getting denied and reimbursement delays. Ultimately, such issues influence the practice’s cash and significantly contribute to the revenue leaks along with other issues. Below is the breakdown:
- Claim denials are due to reasons such as coding errors, incomplete documentation, lack of medical necessity, or eligibility issues.
- Inaccuracy and insufficient documentation lead to denials and reduced reimbursement rates.
- Unrecorded or unpaid bills for services and procedures also reduce revenue levels.
- Lack of proper claims follow-ups and denied or incomplete claims also cause revenue leaks.
- Lack of staff training and knowledge of current trends and billing updates also cause revenue discrepancies.
Prevent Revenue Leakage with Expert credentialing & medical billing solutions
Research shows that up to 90% of claim denials are preventable, with credentialing errors and billing inefficiencies being significant contributors. Hence, the expert-driven integration of credentialing and medical billing solutions can help providers retain revenue levels and ensure operations efficiency.
These may include automation for effective tracking of billing and financial performance. Automation in provider enrollment and credentialing processes helps reduce the lengthy processing time while ensuring compliance and faster approvals. On the other hand, manual credentialing causes 50% of provider delays, increasing the risk of revenue fluctuations. However, automation in credentialing keeps providers updated on applications and status payments.
As for billing improvement, the professionals should focus on tasks like maintaining pricing integrity by offering flexible payment options based on the value your practice provides. Plus, automated tracking helps professionals monitor and record many expenses in the billing process. There are also other key factors as follows:
- Focus on effective AR (accounts receivables) follow-ups for reimbursement and underpayments.
- Make sure your administrative staff is aware of the protocols and standards to engage consistently with payers.
- Make periodic reports to disclose any missed or non-calculated short payments.
- Your practice should have a dedicated workforce that works precisely and pays detailed attention to patients.
- Your practice workforce should have specific expertise to deal with credentialing efforts and critical complications.
- Make sure your practice staff meets the provider-payer pre-defined compliance criteria for a seamless reimbursement flow.
- Avoid the usage of non-compliant and outdated practice management software for your billing and revenue cycle management.
- Ensure end-to-end assessment and audits of your practice’s revenue cycle management (RCM).
Follow TheCredentialing’s structured auditing and assessment for your practice cash flow improvement and revenue cycle that follow the standards of USA medical billing services. Our experts audit and review the claims before their filing. We cover the category of physician specialties practicing under different payment models.
Medical Billing Trend on Rise
With the growing phase of the healthcare industry requiring more focus on efficiency and accuracy in practices, tech trends have taken the lead in medical billing, shaping the future for professionals. Apart from managing claims, medical billing has become the entire ecosystem of financial health to ensure healthcare professionals are comprehensively compensated for the services they deliver. See what the trends are on the rise in medical billing to ensure the fine line for revenue cycle management.
Automation and AI in medical billing
Automation and artificial intelligence (AI) have significantly covered the ground in healthcare medical billing by streamlining many tasks. For instance, claim submission, denial management, and payment posting through robotic process automation (RPA). Automation has increased the efficiency of the practice in tasks like streamlining manual efforts.
Predictive analytics technology integration helps providers detect errors in billing and identify the claims that are likely to get denied. These identification tools help professionals take the necessary steps earlier to make improvements in claims and billing.
Data analytics for real-time results
Since healthcare providers are in need to analyze large amounts of data, errors are inadequate. Utilizing real-time data analytics ensures real-time results for immediate financial and care outcomes. Such tools offer information about claims’ progress, patients’ payment behaviours, and payment trends. So that the providers make crucial adjustments in RCM strategy to improve medical billing.
Healthcare’s tendency towards patient-centric billing
Patients requiring ease, transparency, and flexible billing significantly influence each step of healthcare providers’ billing tasks. Such a patient-centric billing approach requires providers to ensure clear and concise communication of financial obligations. For instance, we can offer patients user-friendly portals, transparent pricing measures, and flexible payment options to add to patient satisfaction.
Investing in effective denial management practices
The industry reports suggest that a significant number of claim denials are caused by incorrect coding, late submissions, and missing information. Investing in effective denial management practices is a must such as automated denial tracking systems. Tracking the issues will offer insights to make the best improvements and avoid denials in the future.
Integration of interoperable systems
The data exchange between the payers, providers, patients and other involved entities is a crucial component of medical billing. For professionals to ensure the accuracy and efficiency of billing, seamless data exchange is due through the integration of interoperable systems. These systems will help providers ensure secure data exchange and streamline processes like prior authorization, eligibility verification, and payment reconciliation.
Outsourcing is always the best in medical billing and credentialing
The integration of many tech trends in billing and credentialing is due, but outsourcing keeps your practice updated with a focus on billing regulations and changing compliance needs.
Ensure that you contract with the expert RCM Medical billing company to turn your practice billing complexities into efficiencies. Outsourcing medical billing will offer effective assistance in reduced overhead costs, access to specialized expertise, and the ability and space to increase patient care quality while limiting the need to mingle with other tasks.
TheCredentialing is an experienced partner to verify your provider’s credentials with due care. Plus, we help your practice expand the insurance network while staying compliant with the payer guidelines and approval requirements. For your government or commercial insurance credentialing, we are here to provide effective automation through our TheCredentialing Digital Portal. Get your credentialing and billing security with complete transparency and efficient management.





